It’s not likely covid-19 will be completely eradicated, at least not any time soon.
That would be the best case scenario, said Dr. Graham Snyder, medical director of Infection Prevention and Hospital Epidemiology at UPMC.
The worst case would be that the virus continually evolves to become more deadly and requires more vaccine development every year.
But more likely, experts say, the pandemic’s end will fall somewhere in the middle, where cases of covid-19 still occur, but they are less deadly and less frequent.
“There’s a high probability it turns into an endemic virus like seasonal influenza,” said Dr. Thomas Walsh, an infectious disease expert at the Allegheny Health Network. “It may well be that we need booster vaccines at certain intervals, yearly or every several years.”
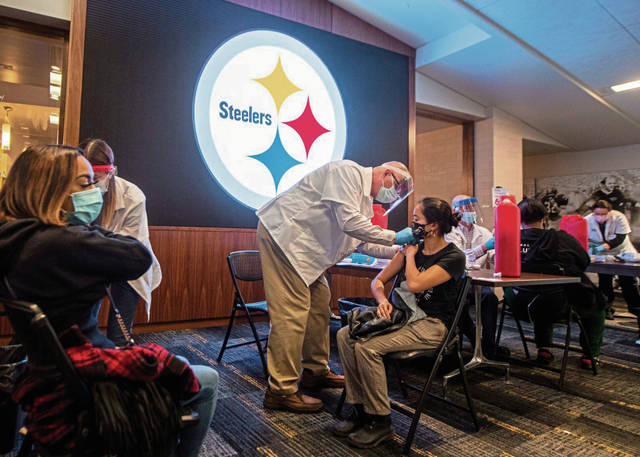
This week marked the one-year anniversary of covid-19 in the Western Pennsylvania region. After surpassing 532,000 deaths nationwide, infections and more than deaths, the virus finally appears to be receding. Case levels, hospitalizations and deaths are trending downward and the vaccine distribution is gaining momentum.
Nevertheless, health experts say it still will take some time for the pandemic to be “over.”
And when it is over, they say, some things will not be the same as they were a year ago.
***
Widespread vaccination is one of the most important factors in relaxing public health mandates and bringing the pandemic to an end, experts say. So are the widespread safety mitigations that have been in place nearly all year.
The development of successful covid-19 treatments and infection prevention methods — ways to prevent transmission, such as mask-wearing and hygiene — will continue to be essential. UPMC is developing drugs using covid-19 antibodies, for instance, which have seen success in trials.
“If we have a treatment that guarantees you would not have a complication from covid,” Snyder said, “that would also be transformative. And that will probably come in the form of monoclonal antibody therapies.”
The vaccines, the treatments and the public health mitigations are already under way.
So when can people expect life to go back to normal?
Since mid-December, inadequate vaccine supply has been the No. 1 factor preventing speedy distribution and widespread protection from the virus. Experts say the availability of a third vaccine, from Johnson & Johnson — one that needs only one shot, rather than two — will change the game in terms of distributing the vaccine quickly. And President Biden said on March 2 that the U.S. should have enough vaccine supply by the end of May — a full two months earlier than he had previously predicted.
Even with the recent milestones, though, it’s unlikely enough people will be vaccinated by this spring to call things normal, experts say. Health leaders and government officials have asked people to continue being cautious, even after they’ve gotten a dose.
“For the foreseeable future — by which I mean months — we’ll still have to mask and distance,” Snyder said. “They will still be really important interventions.”
Walsh noted that having enough vaccines is still different from having the ability to actually vaccinate people. But nonetheless, by the end of summer, it’s widely expected there will be more than enough for everyone in the United States.
And with warmer temperatures and more outdoor events, where transmission is also reduced, life could look more normal.
It’s possible there could be another wave of infections next fall or winter, thanks to colder temperatures, some experts predict.
But with widespread vaccination and herd immunity, many predict the cases will be less severe or isolated to individual outbreaks. Health professionals and public officials alike are feeling more optimistic.
“There’s light at the end of the tunnel, and that light seems to be getting brighter,” Allegheny County Executive Rich Fitzgerald said at a news briefing in February.
***
Still when the pandemic does end, “normal” probably will look different in a number of ways.
Mari Webel, an assistant professor of history at the University of Pittsburgh, said someone first asked her to make a prediction about the end of the pandemic, based on her historical knowledge, last June.
She’s a specialist in the history of public health, teaching a variety of courses relating to health controversies in history — especially analyzing the way infectious disease epidemics intersect with politics and social change. She addresses topics such as the problem and politics of quarantine, vaccine hesitancy and a litany of other medical concepts that are now parts of society’s broader vocabulary.
Studying past epidemics help policymakers ask better questions in the future, understanding what’s been successful and ultimately making humanity better at solving problems, Webel said. Covid-19 will be no different.
Historians, public health researchers and experts in other disciplines will continue to monitor the virus’ effects on life, politics and economics for years to come. Covid-19, specifically, highlighted striking inequities in schools, neighborhoods, health care and beyond, as low-income individuals, essential workers and communities of color were disproportionately affected by the virus and shutdowns.
“We will absolutely be able to learn from this experience,” said Webel, the author of “The Politics of Disease Control,” which examined sleeping-sickness epidemics in Eastern Africa, and co-author of a 2020 article explaining the similarities and differences between covid-19 and influenza pandemics. “How we take what we learn and implement it in the future, I think, is an open question.”
“There are just ways of thinking about things that are shifting,” she added.
Walsh said scientific research will continue — health professionals will only learn more about covid-19 variants, treatments and vaccines. He compared it the SARS outbreak in 2003 — which researchers are still studying today.
“I think there are lessons that we could learn about general hygiene and mitigation strategies,” Walsh said. “Mask-wearing during influenza season or when you are sick is … something that has proven effective that we had poorly studied before.”
But the lessons won’t just be related to public health needs or general infection prevention. Educators say they see a return to school buildings without more widespread use of technology in lessons as unlikely — teachers probably will continue using Google Classrooms, asynchronous lessons and other methods developed out of necessity in the last year.
Some superintendents say remote learning has opened up new options for students who are sick with a non-covid illness — they no longer have to power through an in-person school day to keep up their attendance record.
One thing is for certain: The way Webel teaches about disease outbreaks — the way her students consider these events in history — will never be the same.
She does one in-class exercise in lessons relating to vaccinations during polio outbreak involving a simulation to help students understand the concept of herd immunity. She doesn’t think she’ll ever have to use that tool again.
“My students, coming into the classroom for at least the next generation of students, are going to have a sense of what community transmission of an epidemic disease looks like,” she said. “They’re going to have a sense on a lot of things.”